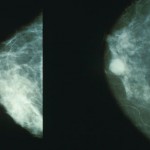
 A new study by investigators at Brigham and Women’s Hospital in collaboration with researchers at the University of York and Leeds in the UK and MD Andersen Cancer Center in Texas puts to the test anecdotes about experienced radiologists’ ability to sense when a mammogram is abnormal. In a paper published August 29 in the Proceedings of the National Academy of Sciences, visual attention researchers showed radiologists mammograms for half a second and found that they could identify abnormal mammograms at better than chance levels. They further tested this ability through a series of experiments to explore what signal may alert radiologists to the presence of a possible abnormality, in the hopes of using these insights to improve breast cancer screening and early detection.
A new study by investigators at Brigham and Women’s Hospital in collaboration with researchers at the University of York and Leeds in the UK and MD Andersen Cancer Center in Texas puts to the test anecdotes about experienced radiologists’ ability to sense when a mammogram is abnormal. In a paper published August 29 in the Proceedings of the National Academy of Sciences, visual attention researchers showed radiologists mammograms for half a second and found that they could identify abnormal mammograms at better than chance levels. They further tested this ability through a series of experiments to explore what signal may alert radiologists to the presence of a possible abnormality, in the hopes of using these insights to improve breast cancer screening and early detection.
“Radiologists can have ‘hunches’ after a first look at a mammogram. We found that these hunches are based on something real in the images. It’s really striking that in the blink of an eye, an expert can pick up on something about that mammogram that indicates abnormality,” said Jeremy Wolfe, PhD, senior author of the study and director of the Visual Attention Laboratory at BWH. “Not only that, but they can detect something abnormal in the other breast, the breast that does not contain a lesion.”
In the clinic, radiologists carefully evaluate mammograms and may use computer automated systems to help screen the images. Although they would never assess an image in half a second in the clinic, the ability of experts to extract the “gist” of an image quickly suggests that there may be a detectable signs of breast cancer that radiologists are rapidly picking up.
In previous work, Wolfe and his colleagues found that radiologists could distinguish abnormal mammograms after a half-second glimpse but that non-experts could not. In the current study, the researchers tested whether breast tissue symmetry, breast density, image size, resolution or other characteristics were contributing factors to the success rate of the radiologists. They found that performance did not depend on breast symmetry or breast density but finer details of the texture of the breast tissue did help radiologists make the correct diagnosis more frequently.
Interestingly, the team found that radiologists could do better than chance in discriminating breast cancer cases from normal tissue, even when the images of abnormal breast tissue did not directly capture a cancerous lesion or when those images were taken from the contralateral breast (the breast on the other side of the body) of a woman with breast cancer.
“These results suggest that there may be something in the nominally normal breast that looks abnormal and is detectable,” said Wolfe. “Together, these results suggest that radiologists may be picking up on some sort of early, global signal of abnormality that is unknown to us at this point.”
Defining the signal that experienced radiologists are detecting could help researchers refine and improve Computer-Aided Detection (CAD) systems that can aid in medical screening and could be incorporated into training for medical experts to improve detection. The team is also interested in exploring whether other medical image experts such as dermatologists and pathologists can use analogous signals.