 A study released on January 6, 2015 from the University of Iowa (UI) has linked: abnormalities of the cerebellum, differences in cerebral white matter, and bipolar disorder.
A study released on January 6, 2015 from the University of Iowa (UI) has linked: abnormalities of the cerebellum, differences in cerebral white matter, and bipolar disorder.
The study, “Brain Abnormalities in Bipolar Disorder Detected by Quantitative Tρ Mapping,” was published in the journal Molecular Psychiatry.
Casey Johnson, PhD, and University of Iowa postdoctoral research fellow was the first author on the study. John Wemmie, MD, PhD, and UI professor of psychiatry was the senior study author.
For this revolutionary study, University of Iowa researchers used a new MRI technique called quantitative T1rho mapping which can provide rapid high-resolution images of the whole brain. This is the first time that neuroscientific researchers have used T1rho imaging to investigate a psychiatric disease.
This new brain imaging technique is a breakthrough. T1rho MRI scans are highly sensitive to specific byproducts of cellular metabolism—including levels of glucose and acidity—that other brain imaging techniques are unable to map in high-resolution.
Conventional imaging tools are generally sluggish, low-resolution, and require that researchers identify what brain regions they want to hone in on at the beginning of the study.
What Is Bipolar Disorder?
Bipolar disorder—which is also sometimes called manic-depressive disorder—is generally characterized by extreme mood swings which range from severe lows of depression to manic highs. About one percent of the general population is affected by a bipolar disorder.
Lithium was approved in the 1970s by the FDA and remains one of the most widely used medications for treating bipolar disorder. Lithium helps reduce the severity and frequency of manic episodes.
Surprisingly, doctors still don’t understand exactly how lithium works to help patients with bipolar disorder. These recent findings from UI offer new clues for solving the riddle of how lithium helps patients with bipolar disorders.
“Whatever the Cerebellum Is Doing, It’s Doing a Lot of It.”
This morning, I had a chance to speak on the phone with Casey Johnson and share my excitement about the new UI study. My fascination with the cerebellum was passed on to me by my father, Richard Bergland MD, who was a neurosurgeon, neuroscientist, and author of The Fabric of Mind (Viking).
Later in his life my father became convinced that neuroscientists and medical professionals were underestimating the psychological and cognitive role of the cerebellum.
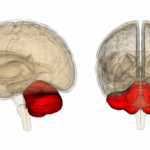
The cerebellum is only 10 percent of brain volume but holds over 50 percent of your brain’s total neurons. Based on this fact, when I was writing The Athlete’s Way (St. Martin’s Press) my father would often say to me, “Whatever the cerebellum is doing, it’s doing a lot of it.” This saying became a mantra for me.
Unfortunately—as a neuroscientific researcher in the late 20th century—the limitations of available brain imaging technology at the time made it impossible for my father to prove any of his “educated guesses” about the cerebellum in his laboratory.
When my father passed away in 2007 I made a vow to follow up on his hunches about the cerebellum and keep my antennae up for advances in our understanding of the cerebellum caused by the advent of technology and better brain imaging methods. Needless to say, this is one reason that I am so excited about this new study and revolutionary MRI technique.
How did the UI researchers discover the link between bipolar disorder and the cerebellum?
On the phone this morning, Casey Johnson reiterated the key points of his new study. Clearly, the high-resolution T1rho imaging gave the researchers a new way to look at “whole-brain changes” as they relate to bipolar disorder.
Interestingly, when Johnson et al set out to compare 15 patients with bipolar disorder and 25 control subjects matched for age and gender using T1rho imaging they weren’t expecting to see the cerebellum light up.
As Johnson describes in a press release, “Our study was essentially exploratory. We didn’t know what we would find,” he adds. “The majority of bipolar disorder research has found differences in the frontal region of the brain. We found focal differences in the cerebellum, which is a region that hasn’t really been highlighted in the bipolar literature before.”
However, when Johnson and his colleagues were comparing the brain imaging of controls without bipolar disorder, they found that in patients affected by bipolar disorder that the MRI signal was elevated in both cerebral white matter and in the cerebellum.
After seeing the cerebellum light up on their MRI scans, Johnson and Wemmie began digging deeper into the scientific literature on bipolar disorder. They were able to cobble together previous research which suggests that the cerebellum may function abnormally in bipolar disorder and that lithium might potentially target the cerebellum and alter cerebellar (of or pertaining to the cerebellum) glucose levels.
Previous studies have linked abnormal cell metabolism with bipolar disorder but investigating metabolic abnormalities with the brain has been limited by rudimentary brain imaging technologies. The UI researchers hypothesize that the elevated signal may be caused by either a reduction in pH or a reduction in glucose concentration.
Is There a Connection Between Cerebellar Volume in Schizophrenia or Bipolar Disorder?
As I was doing more research on the link between the cerebellum and bipolar disorder this afternoon I stumbled upon a study from November 2014 that compared the cerebellar volume in patients with schizophrenia and bipolar disorder.
The research was led by Josselin Houenou (INSERM, Créteil, France). The objective of the study was to compare cerebellar volume between patients with bipolar disorder, patients with schizophrenia, and healthy controls. In addition, the researchers looked at the influence of psychotic features on cerebellar size in patients with bipolar disorder.
The study, “Cerebellar Volume in Schizophrenia and Bipolar I Disorder With and Without Psychotic Features,” was published in the November 2014 journal Acta Psychiatrica Scandinavica.
Houenou and colleagues found that bilateral cerebellar cortical volumes were smaller in patients with schizophrenia compared with patients with bipolar I disorder and healthy controls. Interestingly, they also found no significant difference in cerebellar volume between bipolar patients with and without psychotic features.
The team concluded that a reduction in cerebellar volume is specific to schizophrenia but that cerebellar abnormalities in people with bipolar disorder seem to be ‘more subtle’ than simply a reduction in cerebellar volume.
Conclusion: Is Gaining a Better Understanding of the Cerebellum the Next Frontier for Neuroscience in the Early 21st Century?
The University of Iowa researchers hope that new insights provided by the T1rho imaging will lead to a better understanding of specific brain abnormalities that underlie bipolar disease. Johnson and Wemmie are optimistic that these findings might lead to more fine-tuned methods of diagnosing and treating bipolar disorders.
In a press release Casey Johnson concludes, “Our paper, with this new technique, starts to bring all these pieces of evidence together for the first time.”
Although lithium can be an effective mood stabilizer for people with bipolar disorder, it has a laundry list of unpleasant side effects.
Senior author John Wemmie concluded, “If lithium’s effect on the cerebellum is the key to its effectiveness as a mood stabilizer, then a more targeted treatment that causes the same change in the cerebellum without affecting other systems might be a better treatment for patients with bipolar disorder.”